By Kent Groves, PhD, Global Head of Health Strategy, Dentsu Health and Head of Dentsu Health, EMEA; Julie Allen, SVP, Senior Client Partner, Merkle Health, a Dentsu Company
In consideration of the anticipated decline in available health professionals and related services to meet the demands of a rapidly aging global population, accelerating engagement with programs that support patients early in their treatment journey are critical. The opportunity to educate, support, monitor and track individual progress via these programs serves to enhance individual quality of life (QOL), reduce excessive system costs (payor, provider), stress (caregiver) and optimize the value and strength of the manufacturer/HCP/patient relationships.
There was a time when “patient adherence” simply referred to an individual’s propensity to stay on therapy, and patient assistance programs were a voluntary value-add to support patient questions and concerns when their usual network of doctors, nurse practitioners and dispensing pharmacists weren’t available, or couldn’t provide key support.
If we advance our adherence thinking with respect to prescription medication, we can quantify and further define it as the percentage of (prescribed) doses taken for a specified period of time (length of therapy). Adherence is thus, the product of persistence and compliance where persistence is the degree to which patients remain on therapy from initiation without a meaningful interruption, and compliance is a measure of the quality of patient behavior (longitudinal) relative to following (adhering to) treatment guidelines over a specific period of time.
Multi-Faceted Impact of (Non) Adherence
With adherence more effectively quantified (the degree to which a patient is able to or willing to follow medical advice) it is easier to see how it is one of the biggest drivers of unnecessary costs (repeat clinical visits, condition exasperation due to failure to adhere to therapy, disease progression, etc) in healthcare today. The IMS Institute for Healthcare Analytics stated that more than $2.7T was spent on healthcare in the US in 2012, and that the avoidable costs associated with higher medical bills due to non-adherence could be as high as $146B (5.4%).
By 2016, the estimated annual cost of drug-related morbidity and mortality resulting from nonoptimized medication therapy had grown to $528B, equivalent to 16% of total US health care expenditures.1 Applying these same metrics to 2021, where total US healthcare spending had increased 50+%2 to approximately $4.1T, the annual cost of drug-related morbidity and mortality resulting from failure to adhere to a prescribed therapeutic regimen had jumped to $615B ($1,900/every US citizen).
While there are many variables that ultimately impact medication adherence, the two largest considerations have to do with the patient: health care professional (HCP) relationship and the timing/impact and quality of communications with the patient/care giver, relative to the therapeutic content of a prescriptive intervention. In effect, robust communications between a patient and their HCP (this group includes clinical support, NP/PAs, Medical Specialists, Reimbursement Specialists, Clinical Administrators and others) can overcome many of the traditional influences on adherence.
HCP-Patient Communications
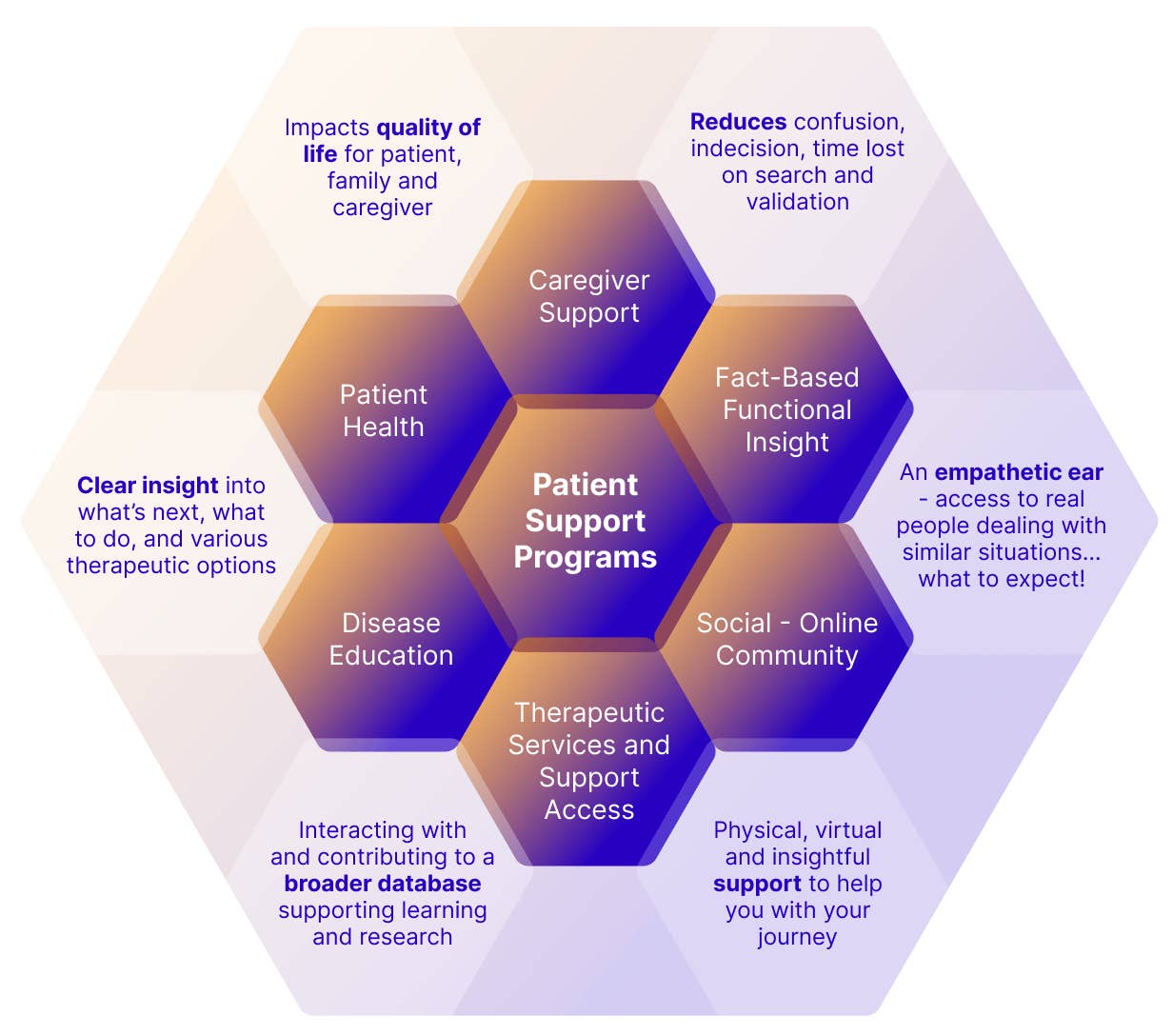
So, while it is really about how well a provider engages and communicates with a patient, today this effort is generally summarized under the broader category of what were once referred to as Patient Assistance Programs, but in recent years have embraced the broader umbrella term of Patient Support Programs (PSP). While the categorization remains the same, when considering the evolving needs of patients and care-givers, PSPs have also evolved from transaction-based assistance to holistic programs that now cover medical education, counseling, financial assistance, clinical interventions, peer support, technology enabled engagement (e.g. AI and remote access) and clinical support and intervention. Consider the broader set of relationships that influence and benefit from PSP facilitated engagement between the health service community and the patient/caregiver outlined in Figure 1.
PSPs: Now, How and Why
Historically, the majority of medication adherence programs have focused on patients who have opted-in to ongoing brand communications. Given the typically low opt-in rates of less than 5%, targeted communications had limited scope, reach and impact. This was due in part to the fact that these communications typically took place well after the initial point of inflection with the HCP, when the seriousness of the condition, value of the medicine and potential side effect direction was top of mind. To significantly impact adherence, and build Rx brand trust and confidence, we need to fortify the initiation of therapy, accelerate access to and acceptance of (PSP) engagement options, and the value of clinical relationships beyond the office visit. Optimizing this opportunity will result in a lift in compliance and persistence that will serve to overcome the gap between prescription and impact.
The value of this engagement goes well beyond what it can do in the short term for the patient, but serves to inform longer term health strategies, both for the individual, caregivers, their HCP and others with similar conditions. The Association of the British Pharmaceutical Industry (ABPI) defines PSPs as an organized system where a marketing authorization holder receives and collects information relating to the use of its medicinal products. Examples are post-authorization patient support and disease management programs, surveys of patients and healthcare providers, information gathering on patient compliance, or compensation/reimbursement schemes.
This (self-reported) insight can be leveraged anonymously (non-identified information) to inform next level programs, establish patient expectations, and inform best practices that can have a significant impact on patient reported outcomes (PRO) and QOL. In effect, serve to better the whole by working to close the proverbial health care gap (the difference between today’s reality and what could be possible).
Learn more or get in touch with Dentsu Health at?



